Disparities in Reproductive and Sexual Health of Individuals with Disabilities
Written By Therese Derovanessian
TLDR: About 12% of U.S. women of childbearing age (7-8 million women) have a physical, hearing, vision, or cognitive disability - most of these women have typical fertility (Horner-Johnson et al., 2018). Therefore, exploring barriers to reproductive & sexual health for women with disabilities is vital to ensure that every woman receives comprehensive healthcare and exercises her rights to personal choices.
Unfortunately, women with disabilities face substantial disparities in accessing reproductive and sexual healthcare compared to their non-disabled counterparts. These disparities are often rooted in issues such as physical inaccessibility, social stigma, limited reproductive and sexual health education, lack of personalized healthcare, and financial challenges.
Through identification and awareness of these barriers, physiatrists can enhance inclusivity, offer education and resources as needed, and provide comprehensive patient support. We can strive to create an inclusive and equitable society where women of all abilities can access service, information, and help to make informed decisions about their reproductive and sexual well-being.
Overview:
Incorrect Assumptions & Lack of Autonomy
Make it stand out
Patients found healthcare providers quick to assume that they do not need contraception as adolescents (Alhusen et al., 2020 & Horner-Johnson et al., 2019).
Women with disabilities are often less knowledgeable about contraceptives than women without disabilities, as shown in a systematic review (Horner-Johnson et al., 2019).
Patients' reliance on caregivers for transportation to appointments creates a barrier to open discussions on sexual activity, sexual health, and family planning options (Alhusen et al., 2020).
One woman with a spinal cord injury described how she felt her mother's presence at her appointment kept her from being able to talk openly about her sexual health (Alhusen et al., 2020).
Falling Short of Inclusivity
Many patients report a reluctance among their healthcare providers to discuss reproductive & sexual health issues during medical appointments, paired with negative attitudes from their care providers (Horner-Johnson et al., 2021 & Horner-Johnson et al., 2019).
For instance, a participant with a spinal cord injury noted, "No one ever asked if I wanted to be pregnant or if I didn't want to be pregnant" (Alhusen et al., 2020).
Furthermore, Alhusen et al. found that a substantial number of participants encountered significant delays in finding a healthcare provider capable of addressing their reproductive needs, especially in the context of their disability.
Physical Barriers
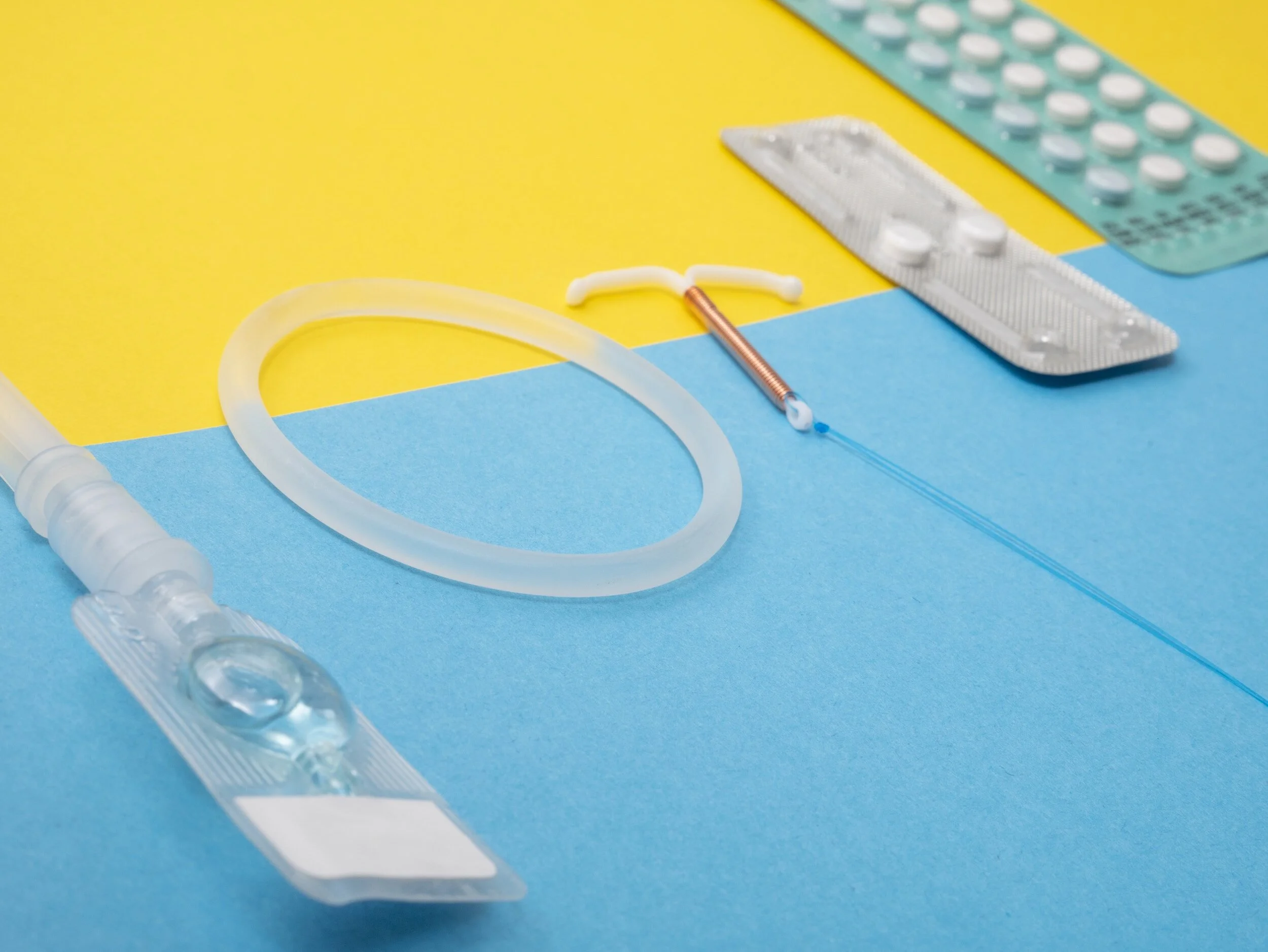
Women with physical disabilities encounter physically inaccessible clinics and exam tables (Horner-Johnson et al., 2021 & Horner-Johnson et al., 2018). For example, women with mobility limitations often cannot tolerate the positioning required for IUD insertion. Women with disabilities affecting their speech or hearing face challenges in communicating with healthcare providers (Alhusen et al., 2020). Women with sensory or intellectual disabilities face challenges with clinical forms & health information (Horner-Johnson et al., 2019).
Contraception side effects impact women with disabilities more severely. For instance, weight gain can further limit mobility, and hormonal birth control can increase the risk of blood clots in patients with paraplegia (Mackiewicz-Milewska et al., 2016).
Some participants have specific disabilities that interact physiologically with specific contraceptives, limiting their options.
Financial Barriers
Women with disabilities face financial challenges that stem from their unique health situations: reduced work opportunities, increased healthcare costs, & need for specialized care or assistive devices.
Patients with disabilities, particularly those with public insurance, face challenges in finding healthcare providers willing to see them (Horner-Johnson et al., 2019 & Horner-Johnson et al., 2022;).
A study found delays in reproductive care due to "...a shortage of healthcare providers who accepted their insurance (i.e., Medicaid)' (Alhusen et al., 2021).
One participant shared her experience, describing feeling "judged" in her interactions within the healthcare system due to her Medicaid coverage. Further explaining that Medicaid limited her options for providers willing to care for her. Sadly, her experience, shared by other participants, ultimately led to an unintended pregnancy due to the delays in finding a provider.
What is part of the solution?
What can PM&R physicians do?
Create a space where patients feel safe to discuss reproductive and sexual health.
Understand that patients need privacy and a space to feel comfortable sharing.
Provide basic reproductive and sexual health education as needed while being aware of which OBGYN colleagues feel comfortable undertaking patients with disabilities for referral.
Be willing to help your patients find someone you recommend within their insurance.
Unique to PM&R
Understand pelvic pain and be aware of differentials, such as recognizing symptoms of endometriosis and OCP-mediated vulvodynia.
Helpful links:
Epidemiology of Pelvic Floor Dysfunction - Sung & Hampton, 2009
References:
Alhusen JL, Bloom T, Laughon K, Behan L, Hughes RB. Perceptions of barriers to effective family planning services among women with disabilities. Disability and Health Journal. 2021;14(3):101055. https://www.sciencedirect.com/science/article/pii/S193665742030193X. doi: 10.1016/j.dhjo.2020.101055.
Horner-Johnson W, Klein KA, Campbell J, Guise J. Experiences of women with disabilities in accessing and receiving contraceptive care. Journal of Obstetric, Gynecologic & Neonatal Nursing. 2021;50(6):732-741. https://www.sciencedirect.com/science/article/pii/S088421752100126X. doi: 10.1016/j.jogn.2021.07.005.
Horner-Johnson W, Klein KA, Campbell J, Guise J. “It would have been nice to have a choice”: Barriers to contraceptive decision-making among women with disabilities. Womens Health Issues. 2022;32(3):261-267. https://www.sciencedirect.com/science/article/pii/S1049386722000019. doi: 10.1016/j.whi.2022.01.001.
Horner-Johnson W, Moe EL, Stoner RC, et al. Contraceptive knowledge and use among women with intellectual, physical, or sensory disabilities: A systematic review. Disability and Health Journal. 2019;12(2):139-154. https://www.sciencedirect.com/science/article/pii/S1936657418302103. doi: 10.1016/j.dhjo.2018.11.006.
Mackiewicz-Milewska M, Jung S, Kroszczyński AC, et al. Deep venous thrombosis in patients with chronic spinal cord injury. J Spinal Cord Med. 2016;39(4):400-404. doi:10.1179/2045772315Y.0000000032